A blog post from medTec Systems
The importance of patient pre-warming to avoid perioperative hypothermia
Despite the increasing number of studies on perioperative hypothermia and the consistent recommendations to pre-warm patient´s inadvertent perioperative hypothermia is still a challenge in the surgical field. Scientists and clinical practitioners agree that patients should be pre-warmed before surgery to ensure normothermia at the beginning of surgery.
Important suggestions on perioperative warming management can be found in the German S3 guideline „Prevention of perioperative hypothermia“ [1] as well as in the UK-„NICE guidelines“ of the National Institute for Health and Care Excellence. [2] However, these documents do not yet take into account newer solutions for hypothermia prevention. This, combined with inadequate knowledge and training on patient thermal management, means that patients repeatedly suffer hypothermia pre-, intra- and post-operatively. According to an American study, the hospital mortality rate for patients with moderate or severe acute hypothermia is 40% despite modern preventive measures. In most cases, perioperative hypothermia is preventable. [3]
We have compiled 5 of the most significant reasons to implement a solid patient warming strategy.
1. Increased well-being of patients
The well-being of patients in the entire surgical environment is the focus of healthcare efforts. Pre-warming leads to better surgical results and reduces the risk of complications. Normothermic patients have a more positive perception of the entire surgical situation. An article by the American Association of Nurses, AORN, states that perioperative heat management can prevent patient discomfort, reduce anxiety and make patients feel better prepared for the upcoming surgical procedure. Warmed patients also fall asleep more quickly when anesthesia is induced. [4]
The well-being of patients improves with preoperative warming regardless of the chosen warming method. Older participants in the study responded better to passive warming measures than younger ones due to their higher body temperature. [5]
Keeping a patient warm before surgery, from the ward to the procedure, increases their well-being. Patients can also lose body temperature during transfers between different treatment units and during extended waiting times. With active warming systems, usually dependent on a power supply, heat gaps can occur when changing location and the patient may arrive at the operating theater cool or hypothermic. Passive warming blankets, pre-warmed when required, reflect the patient’s own body heat from the ward to the operating theatre and also keep the patient warm throughout the entire surgical procedure.
2. Reduced complications
According to an article in the Journal of Perioperative Nursing, approximately 70% of surgical patients experience inadvertent perioperative hypothermia – far too high a number for a preventable problem. [6] Many studies have shown that, depending on the condition and age of the patient, inadvertent perioperative hypothermia can cause a variety of complications including cardiac arrhythmias, infections, prolonged bleeding, shivering and even increased mortality. Hypothermic and shivering patients consume more oxygen, may require more pain medication, have a longer recovery time and longer hospital stays. [4]
3. Cost efficiency
With the reduction in complications and faster recovery times also the post-operative stay of patients in hospital can be shortened. This reduces costs for staff, beds, medication, food, textiles and much more. Further savings are achieved through the use of passive warming blankets. An internal study by the Orthopedic Hospital NHS Trust comparing passive and active air-warming systems found savings of GBP 13 (approx. USD 17) per surgery for the use of passive warming blankets. Given the annual number of surgical interventions a hospital performs, this adds up to a significant cost block.
The costs induced by perioperative hypothermia are a massive burden for many national healthcare systems. The study „Costs of inadvertent perioperative hypothermia in Australia: A cost-of-illness study“ estimates the annual cost of inadvertent perioperative hypothermia to the Australian healthcare system at over AUD 1.25 billion (approx. USD 761 million). It is recommended that measures to prevent inadvertent hypothermia should be intensified, with a particular focus on pre-warming patients. Detailed model calculations show dramatic cost savings. [7]
4. Improved surgical outcomes and resource utilization
Surgical procedures come with a variety of risks, therefore, reducing as many risks as possible is key to improving the patient’s outcome. Influencing factors such as anesthesia, state of health, temperature in the preoperative room and operating room and other parameters, as well as their combination, can lead to inadvertent intraoperative hypothermia. [8] In particular, hypothermia impairs the immune defense of hospital germs. Hypothermia typically will develop within the first hour of surgery, usually after induction of anesthesia. This is particularly problematic during long surgical procedures.
According to a systematic review on perioperative hypothermia, hypothermia is the least monitored complication of anesthesia and surgical procedures. The core temperature of non-prewarmed patients dropped more during surgery than the core temperature of prewarmed patients despite active warming. It is recommended to start hypothermia management 1 to 2 hours before induction of anesthesia. [3] Surgical procedures become even more challenging with an ageing population. Older people are more at risk of complications during operations such as fall-related hip fractures. Preoperative warming of patients is a simple and effective measure to reduce unnecessary subsequent risks of perioperative hypothermia.
5. Saves resources and reduces waiting times
Even in post-Covid times, there are still delays before surgical interventions. Pre-operative warming saves additional waiting time and spares resources in the operating room, on the ward and shortens the post-operative stay. This frees up the bed for the next patient and improves the flow on the list for surgeries.
Our solution: Passive hypothermia warming blankets
There are a variety of warming methods, each with their own benefits and drawbacks. Passive warming blankets are a cost-effective, space-saving and practical solution that makes patients feel comfortable.
Active warming systems with air blowers have been used in hospitals for decades and have been proven to achieve positive results. However, compared to passive warming blankets, these systems are costly in purchase as well as more expensive labor-intensive to run. They can be the method of choice for long surgical procedures, but can also entail risks such as contamination of the surgical site [6] or expose surgical staff to unwanted warming.
Blankets made of cotton or microfleece are often used. However, even if these blankets are pre-warmed they become ineffective within a few minutes due to their low heat storage. In order to keep a patient warm in this way, a large number of blankets would be needed. This is not time or cost efficient. [6]
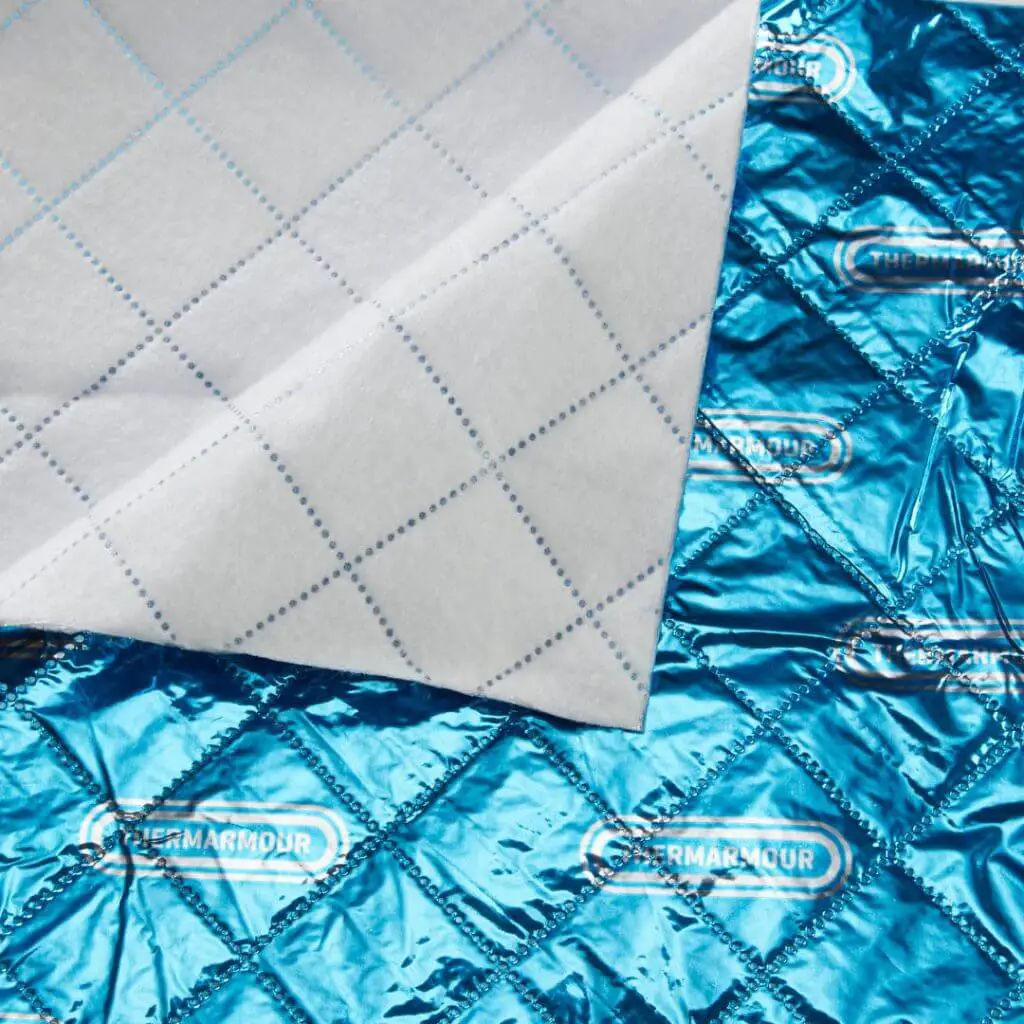
Comparatively, warming blankets with passive thermal technology act like an insulator. They absorb almost all the body heat released and form a long-lasting thermal envelope around the body. In addition, the passive warming blanket can accompany the patients throughout the surgical procedure and keep them warm continuously.
However, not all passive warming products are created equal. There are different types of „foil blankets“ and not all of them are suitable for medical use. Thin conventional foil blankets do not provide the insulation and stability required for surgery. Multi-layer composite blankets offer insulation, robustness and patient comfort combined.
The multilayer warming blankets offered by medTec Systems have been developed over many years in collaboration with clinicians and independent experts, have been thoroughly tested and have proven themselves in clinical practice.
Stay in touch and learn more about our products, clinical evidence and new developments.

Physiotherapy heat treatment

Physiotherapie Wärmebehandlung

Patienten Vorwärmung